Prevention of Retinal Detachment
Rhegmatogenous retinal detachment (RRD) is a well-recognized risk factor for detachment in the fellow eye. Before the 20th century, RRD was suddenly blinding to the affected eye and often bilaterally blinding due to subsequent RRD in the second eye. We now have reasonably successful cures for RRD, but after a half century of trying retinal surgeons have still not developed effective prophylaxis.1 Although it is not widely recognized, fellow eyes of patients with bilateral pseudophakia and first eye detachment suffer an RRD rate of approximately 26%, 2, 3 probably constituting the largest group of asymptomatic eyes at high risk of RRD. This is especially important to patients who have suffered loss of macular function in the first eye and for whom a second RRD could be catastrophic.
Because most causative tears in these fellow eyes have been reported to occur in normal-appearing peripheral retina,2 we have applied encircling laser prophylaxis with the indirect ophthalmoscope (IDO), reducing the RRD rate in pseudophakic fellow eyes from an average of 19% with no treatment or focal treatment to 1.4% (P<.001), with an average follow-up of 5 years. This pilot study of 269 pseudophakic fellow eyes was presented at the 2002 combined meeting of the Retina Society and the American Society of Retina Specialists (ASRS).
4 Based on this experience, and similar results in other eyes at high risk of RRD, we believe that producing a “second ora” (ora secunda) posterior to the at-risk peripheral retina by laser cerclage (ora secunda cerclage [OSC]) is the first reported retinopexy treatment that can reliably protect eyes known to be at high risk of RRD. This report provides an overview of this study, pending further analysis and the additional follow-up needed for a final report.
FOCAL PROPHYLAXIS
While much has been written on the subject of RRD prophylaxis, the literature still lacks randomized, controlled trials. We do have the benefit, however, of a comprehensive literature review by the American Academy of Ophthalmology Preferred Practice Patterns committee.1 This review found that focal treatment of asymptomatic holes, tears, and lattice degeneration was not supported with data of significant strength. Retinopexy treatment of asymptomatic predisposing lesions appears to be effective at preventing RRD emanating from the treated lesions, but too often new tears occur in normal-appearing retina between treated lesions (Figure 1).
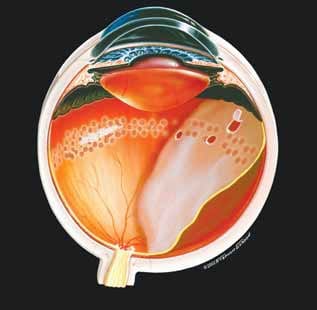
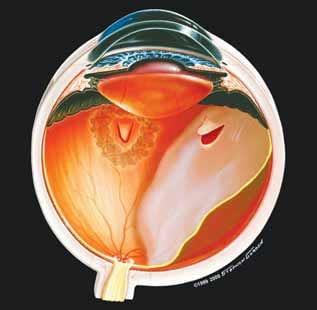
Figure 1 Figure 2
In one frequently cited study 1,2 of fellow eyes undergoing cataract extraction, focal treatment of all visible lesions in 124 fellow eyes would have prevented only two of 21 subsequent detachments, because 19 of the 21 detachments (90%) were caused by new breaks in normal appearing peripheral retina. Byer,5 noting that 89% of detachments in untreated eyes with two or more risk factors arise from normal appearing areas, concluded that “if we cannot predict the danger sites, we cannot prevent detachment.”
ENCIRCLING LASER PROPHYLAXIS BY SLIT-LAMP DELIVERY
While it is true that we cannot predict the meridian of a future break, we can predict that most causative breaks will occur in the peripheral retina. This led physicians in Israel and France in the 1970s and 1980s to perform an equatorial “fence” of encircling laser prophylaxis, posterior to the at-risk peripheral retina. Even after these slit-lamp–based treatments, however, breaks anterior to treatment could still cause RRD, and iatrogenic breaks also occurred at sites of laser treatment, as the retina separated from the treated pigment epithelium (Figure 2).
This encircling laser prophylaxis was not widely adopted and was often considered to be ineffective and even harmful.6 The net result was to discredit the concept of encircling laser prophylaxis as a rational answer to focal prophylaxis failure, even as a substantial technical advance in laser treatment was about to appear.
ORA SECUNDA CERCLAGE (OSC): CREATING A SECOND ORA
The IDO laser delivery system became clinically available about 1990. The IDO allows the same advantages for peripheral laser treatment that it had earlier brought to retinal diagnosis—widefield viewing of the periphery to the ora serrata, stereopsis, and dynamic viewing by simultaneous scleral depression. As early adopters of IDO laser delivery, we recognized its potential to create a new and more effective form of prophylactic laser cerclage.
Indirect ophthalmoscope laser cerclage allows the comparatively easy delivery of a grid pattern of laser retinopexy from the ora serrata to the vicinity of the equator or more posteriorly if focal lesions dictate. IDO laser cerclage thus creates an “ora secunda,” which we define as the posterior edge of encircling laser retinopexy, placed from the equatorial area to the ora serrata, effectively bonding the entire at-risk peripheral retina to the eye wall. It is technically possible to deliver such a treatment pattern by slit lamp or by endoprobe, but with more difficulty than with the IDO laser.
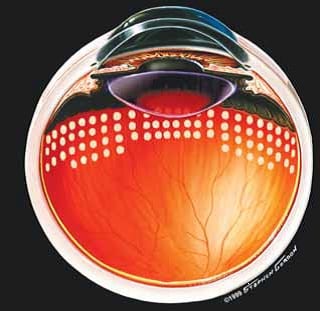
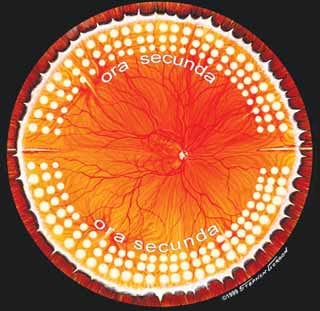
Figure 3 Figure 4
A grid of laser burns of moderate intensity is placed, using one spot width separation (Figure 3). The goal of treatment is to take the at-risk peripheral retina completely “off the field” and “out of play.”
The posterior edge of treatment may be adjusted from eye to eye or even in different meridians at the discretion of the treating physician to incorporate focal pathology, but it should always extend posterior to the vitreous base. Coalescent treatment is given around focal defects or lattice. The 3-o’clock and 9-o’clock meridians are avoided to spare the long posterior ciliary nerves (Figure 4). A typical OSC treatment comprises between 800 and 1,200 spots. Scleral depression technique is particularly important in applying treatment evenly and completely. OSC treatment may be accomplished in the office with retrobulbar injection, or in the operating room with retrobulbar injection laryngeal mask anesthesia, or general endotracheal anesthesia.
RESULTS
At the 2002 combined Retina Society/ASRS meeting, we reported results of a nonrandomized study of 269 pseudophakic fellow eyes in which, after informed
consent, the bilaterally pseudophakic patients were offered observation, focal prophylaxis, or OSC prophylaxis if lattice or defects were noted in the fellow eye; no treatment if the fellow eye had no lesions and the first eye regained good visual acuity; and no treatment or OSC if no lesion was seen in the fellow eye but the first eye lost substantial macular function. Although this is rarely mentioned in the literature, we believe that first eye visual status is a valid consideration for the prophylaxis decision in the second eye. With an average follow-up of 36 months, 33 of 175 untreated fellows eyes (19%) experienced RRD, and five of 22 focally treated fellow eyes (23%) experienced RRD. Only one of 72 fellow eyes (1.4%) receiving OSC experienced RRD in a follow-up period averaging 5 years (P<.001). We have also used OSC with good results in other high-risk settings, such as in vitrectomy for retained lens particles or macular hole, and for patients with extreme myopia who are undergoing lens extraction.
OSC COMPLICATIONS
In OSC procedures, temporary iris sphincter and/or accommodative paresis is occasionally seen. But with grid pattern, moderate intensity, and spared horizontal meridians, these have not been substantial problems. Subjective reduction of peripheral visual field has also been rare. Clinically significant epimacular proliferation occurred in two of 72 eyes (2.7%) receiving OSC, with final acuity of 20/20 and 20/30.
CONCLUSION
A prophylaxis similar to OSC is commonly used by retinal surgeons intraoperatively7-10 to prevent postoperative detachment. Our contribution has been to
introduce the concept of an “ora secunda,” and to introduce OSC as a pure prophylaxis in high-risk eyes that have not yet experienced RRD, demonstrating that it may be reasonably safe and effective with long-term follow-up. In our experience, OSC not only prevents most retinal detachments, but also the occurrence of a retinal tear in the treated area or at its posterior edge is rare. If OSC prophylaxis ultimately proves to be the first safe and effective prophylaxis for asymptomatic, high-risk eyes, it would drive a greater effort to quantify risk factors and to quantify risk for particular eyes. Limitations of this study include treatment based upon informed patient preference rather than randomization and absence of posterior vitreous detachment analysis in the fellow eyes. We intend to soon report this study in detail and with 10 years follow-up in the peer reviewed literature. Level I evidence of OSC safety and effectiveness 1 will require a randomized, controlled trial, which is now in design. Interested physicians are invited to contact us with suggestions or comments, or to participate.